The Ultimate Travel Guide to Ladakh: PART 4 – Comprehensive Guide on Acute Mountain Sickness (AMS)
The Ultimate Travel Guide to Ladakh
PART – 1: Complete Planning Guide
PART – 2: A Breathtaking Journey Via Srinagar to Leh Highway
PART – 3: Exploring Leh, Nubra and Pangong
PART – 4: Comprehensive Guide on AMS
Introduction: Why AMS Matters in Ladakh
Planning a Ladakh trip? Remember—Ladakh is not just another hill station like Shimla, Manali, or Srinagar. It is a spectacular yet demanding destination. The high-altitude terrain requires respect, and ignoring precautions can spoil your holiday.
Imagine reaching Leh, ready for breathtaking views and thrilling adventures. Instead, within hours, you face headaches, nausea, or fatigue. This is a common reality for travelers who ignore Acute Mountain Sickness in Ladakh.
AMS does not discriminate. It can affect anyone, regardless of age, fitness, or lifestyle. Severe cases may become life-threatening, while even mild symptoms can disrupt travel plans and force early descent. Therefore, listen to experts, not those who dismiss AMS because they were lucky to avoid it. With proper acclimatization, you can safely enjoy Ladakh like thousands of travelers do each year.
Understanding Acute Mountain Sickness in Ladakh
What Is AMS?
Acute Mountain Sickness (AMS) occurs when the body struggles to adapt to low oxygen levels at altitudes above 2,500 meters (8,200 feet). Symptoms begin as mild discomfort but can progress into serious, life-threatening conditions if ignored.
Mild Symptoms
- Headache
- Nausea or vomiting
- Fatigue or weakness
- Dizziness
- Insomnia or disturbed sleep
- Loss of appetite
- Shortness of breath on exertion
Severe Symptoms (HAPE / HACE)
If mild AMS is ignored, it can escalate to:
HAPE (High-Altitude Pulmonary Edema): Breathlessness, chest tightness, frothy sputum, bluish lips.
HACE (High-Altitude Cerebral Edema): Severe headache, confusion, hallucinations, loss of coordination, coma.
Why Oxygen Levels Drop at High Altitudes
As altitude increases, atmospheric pressure decreases. Oxygen concentration in the air stays at 21%, but the partial pressure of oxygen (pO₂) reduces.
- Sea Level (0 m): pO₂ ≈ 160 mmHg
- Leh (3,500 m): pO₂ ≈ 104 mmHg
- Khardung La / Chang La (5,500 m): pO₂ ≈ 74 mmHg
At 3,500 meters, only about 60–65% of sea-level oxygen is available. At 5,500 meters, it drops to nearly 50%. This “thin air” challenges the lungs and bloodstream, leading to hypoxia (low blood oxygen), which triggers AMS.
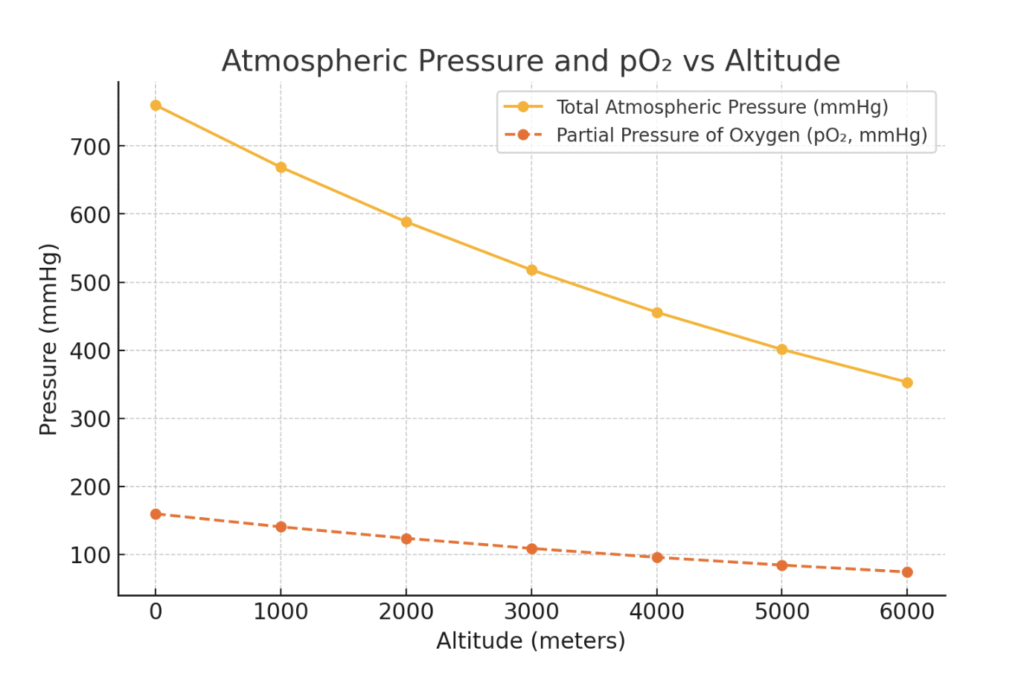
This reduction in pO₂ limits the oxygen available for the lungs to absorb. Put simply, at higher altitudes the air becomes “thinner,” and every breath delivers fewer oxygen molecules. At 3,500 meters (about 11,500 feet), only about 60–65% of sea-level oxygen is available, while at 5,500 meters (about 18,000 feet), it drops further to nearly 50%.
When the body encounters this thinner air and reduced oxygen supply, it begins a series of adaptive responses. These adjustments are complex and unfold gradually, often over hours to weeks. However, rapid ascents can overwhelm the body’s capacity to adapt, preventing proper acclimatization. As a result, oxygen absorption falls short, leading to hypoxia (low blood oxygen levels), which disrupts normal functions and can trigger Acute Mountain Sickness in Ladakh.
How the Body Acclimatizes
Immediate Response (Minutes to Hours)
Hyperventilation: Faster breathing to absorb more oxygen.
Respiratory Alkalosis: Excess CO₂ expelled, blood becomes alkaline. Kidneys compensate by excreting bicarbonate.
Increased Heart Rate: Faster circulation of oxygenated blood.
Early Acclimatization (Hours to Days)
Higher Hemoglobin Production: Kidneys release erythropoietin (EPO), increasing red blood cells.
Oxygen Dissociation Shift: More 2,3-BPG helps hemoglobin release oxygen efficiently to tissues.
Long-Term Acclimatization (Days to Weeks)
More Capillaries: Improves oxygen delivery.
Efficient Mitochondria: Better energy extraction.
Normalization of Heart Rate and Breathing: Body adapts to low oxygen levels.
Why 48 Hours in Leh Is Essential
Most travelers need 24–48 hours in Leh (3,500 meters) for initial adaptation. Light walks after 24 hours are helpful, but avoid exertion.
Road via Srinagar: If you halt overnight in Kargil (2,676 meters), 24 hours may work. Yet, 48 hours in Leh is safer before climbing to Khardung La (5,359 meters).
Individual Differences: Some require 72 hours or more depending on age, medical history, and fitness.
Recent High-Altitude Visitors: They may acclimatize faster but should still take precautions.
Recommended 48-Hour Routine
Day 1: Complete rest. Avoid alcohol, smoking, and heavy meals. Stay hydrated but not overhydrated. Take Diamox if prescribed.
Day 2: Light activities in Leh town, gentle walks, continue hydration and diet precautions.
After 48 Hours: Short trips to lower-altitude areas (e.g., Sham Valley). Delay high-altitude travel until Day 3.
Safe Altitude Gains After Leh
Nubra Valley (3,000 m / 10,000 ft): Generally safe after Leh acclimatization.
Pangong Lake (4,250 m / 13,900 ft): Manageable for most travelers after 48 hours in Leh.
Tso Moriri (4,575 m / 15,000 ft): Requires at least 72 hours of acclimatisation at Leh.
AMS Symptoms by Altitude
High Altitude (8,000–12,000 ft): Mild symptoms may appear.
Very High Altitude (12,000–18,000 ft): Careful monitoring needed. Risks of AMS increase.
Extremely High Altitude (18,000+ ft): Known as the “Death Zone.” Even acclimatised individuals face serious risks.
Common Misconceptions About AMS
Fitness prevents AMS: False. Even fit trekkers can suffer.
Past experience guarantees immunity: No, AMS can recur.
Small descent is enough: Not always; significant descent may be required.
Hydration prevents AMS: Helpful but not foolproof.
Oxygen cures AMS permanently: Only a temporary relief.
Only trekkers get AMS: Tourists are equally vulnerable.
Prevention and Precautions
Golden Rules
Spend two nights at 10,000 ft (3,000 m) before climbing higher.
Limit altitude gain to 300 m per day after 10,000 ft.
Rest for one extra night every 1,000 m gain.
Follow the “climb high, sleep low” strategy.
Pre-Trip Preparation
Plan gradual ascent.
Schedule 48-hour acclimatization at Leh.
Consider hypoxic training tents.
Consult a doctor if you have health issues.
Carry essential medicines, pulse oximeter, and portable BP monitor.
Keep buffer days in your itinerary.
Precautions During Travel
Avoid alcohol, tobacco, and excess caffeine.
Eat light, high-carb meals.
Stay hydrated but avoid overhydration.
Do not overexert.
Stay active during the day, avoid long naps.
Use portable oil heaters instead of electric coil heaters.
Monitor AMS symptoms closely, especially at night.
Carry portable oxygen cylinders if available.
High-Risk Groups Who Should Avoid Altitudes Above 10,000 ft
Heart & Lung Conditions: COPD, asthma, pulmonary hypertension, coronary artery disease.
Blood Disorders: Sickle cell anemia, severe anemia (Hb < 8).
Neurological Issues: Epilepsy, severe migraines.
Pregnant Women: Higher risk of complications.
Infants below 6 months and elderly people with hidden conditions.
Severe Obesity (BMI > 40): Aggravates breathing difficulties.
Recently Ill or Operated Patients: Need recovery time before high altitude.
Those with prior severe AMS, HAPE, or HACE.
Precautionary Measures
Consult a doctor before travel.
Use acetazolamide if prescribed.
Avoid exertion, alcohol, and heavy meals.
Carry oxygen and monitoring devices.
Handling AMS on the Spot
Immediate Actions
Stop ascending.
Rest, stay warm, and hydrate.
Take Diamox if prescribed.
Descend 300–1,000 meters if symptoms worsen.
Emergency Measures
For HAPE or HACE, descend at least 1,000 meters.
Provide supplemental oxygen.
Use hyperbaric chambers if available.
Seek urgent medical help.
Conclusion: Safe Travel in Ladakh
Acute Mountain Sickness in Ladakh is real, but it should not stop you from experiencing this majestic region. Respect altitude, follow acclimatization rules, and prepare wisely. By doing so, you can enjoy Ladakh’s raw beauty, from Nubra to Pangong, without compromising your health.
For a complete trip plan, read our detailed Ladakh travel guide .
For medical resources, refer to the Institute for Altitude Medicine.